SCSA. Spermatozoa are stained with specific dye and a special scanner is used to detect sperm with fragmented DNA. This method is used quite widely and is considered to be one of the most precise methods.
Male Infertility
Infertility is a disease defined by failure to achieve pregnancy after 12 months of unprotected sexual intercourse. Recent scientific researches have revealed that millions of couples all over the world are faced with various disorders influencing fertility. Every sixth or seventh couple trying to conceive a child runs into fertility issues, and in case of every second couple, the problem lies solely in the male partner.
Based on the data of the World Health Organization (WHO), normal sperm count has dropped fourfold since 1990, i.e. from 60 million sperm per milliliter in 1990 to 15 million sperm per milliliter in 2010. Presumably, fertility issues due to the male factor will only multiply in the future.
“Every sixth or seventh couple trying to conceive a child runs
into fertility issues, and in case of every second couple, the
problem lies solely in the male partner.“
Infertility may be categorized under male or female infertility and also as primary or secondary infertility. Primary infertility refers to couples who are unable to conceive a child at all, while secondary infertility refers to couples who have been able to get pregnant at least once but are unable to conceive more children. In this case, the statistical data is once again disconcerting as secondary infertility has been steadily rising in frequency, resulting in the assumption that cases of male fertility are becoming more frequent as well.

Known Causes of Male Infertility
In 2015, the European Association of Urology published Guidelines on Male Infertility. The methods identified in the said Guidelines have been used by a number of urologists and andrologists who specialize in the treatment of male factor infertility.
Known male infertility causes comprise more than half of the underlying reasons of male infertility. Varicocele accounts for the majority of infertility cases and is closely followed by cryptorchidism (undescended testis), erectile dysfunction, disorders of ejaculation, hypogonadism, etc.
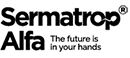
Varicocele is an abnormal enlargement of the veins in the scrotum. This health disorder is present in every sixth infertile male. Most often, varicocele affects the left testicle due to anatomical peculiarities; however, the underlying causes of the varicose vein process are still unidentified. Varicocele is accompanied by blood circulation disorders in the testicles, deficiency in oxygen and nutrient supply and metabolite elimination failure, all leading towards the development of inflammatory processes. Consequently, inflammation inducing substances are discharged and free radicals are produced, resulting in oxidative stress that negatively affects spermatogenesis (the process in which sperm cells are produced and grow mature). The oxidative stress and its effects are discussed in more detail in the next chapter. Usually, no distinct symptoms accompany varicocele, though men may feel a sense of discomfort and stretchiness or other symptoms. Varicocele is diagnosed by palpation.The usual course of treatment of varicocele is surgical and involves either vein ligation and stripping or sclerotherapy. However, the matter of varicocele treatment increasing male fertility is still under heavy debate.
Infertility due to obstruction problems manifests as the absence of spermatozoa in ejaculate (obstructive azoospermia). Usually, obstructive azoospermia originates from inflammation following an infection and/ or trauma. Obstructive azoospermia is diagnosed by performing a semen analysis, hormone balance test and ultrasound. In such a case, surgical treatment is the usual course of action.
Cryptorchidism (undescended testis) is another rare cause of male infertility. In most cases, it is unknown why the testicles fail to descend properly. The disorder is diagnosed in childhood and treatment is prescribed as early as possible. The general course of action is to apply treatment with gonadotropin-releasing hormone.
Erectile dysfunction and disorders of ejaculation. The underlying causes of erectile dysfunction or disorders of ejaculation may vary, e.g. blood vessel pathology, blood circulation disorder in pelvis minor or psychological disorders. Medication and other substances to treat erectile dysfunction are most usually prescribed in such cases.
Sperm antibodies. It is possible for the male body to develop antibodies to own cells, in this case the spermatozoa which later become damaged or killed. Sperm antibodies may be produced due to traumas, infections, etc.
Other yet unmentioned causes of infertility may also include hypogonadism, various genetic disorders, malignant processes, etc.
Idiopathic Male Infertility
Idiopathic male infertility includes all such disorders for which no medical cause for infertility can be ascertained. The disorder is diagnosed when all other clear medical causes are rejected. Idiopathic male infertility is most probably the most frequently diagnosed infertility-associated disorder as almost every third case of male infertility is of unascertained origins. The underlying reasons influencing the development of idiopathic male infertility, aka infertility of unascertained cause, may vary greatly; however, they may also possibly lie in our surroundings and our lifestyle. been used by a number of urologists and andrologists who specialize in the treatment of male factor infertility.
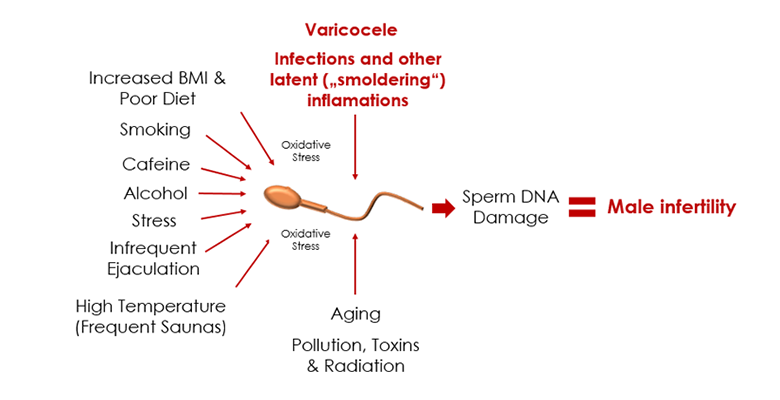
Such negative environmental factors as air pollution, radiation, toxins, unhealthy lifestyle (constant stress, smoking, alcohol abuse, obesity, low physical activity, and inadequate nutrition), inflammatory foci following infections that have not been properly healed and prostatitis give way to oxidative stress which negatively affects the production and maturation process of the spermatozoa.
Oxidative Stress and its Impact on Male Infertility
The chapter is focused on defining oxidative stress and reviewing its key causes and effects on male fertility.
Oxidative Stress and Its Key Causes
Oxidative stress is essentially an imbalance of the reactive oxygen species, also known as free radicals, when overproduction of the latter occurs due to some unknown reason and the natural defense mechanisms of the body lose their ability to counteract or neutralize the amounting surplus of the free radicals. Presumably, as many as 80% of male infertility cases originate from oxidative stress (Tremellen 2008).
As previously mentioned, the generation of oxidative stress is largely influenced by negative environmental factors, unhealthy lifestyle and inflammatory processes in the urogenital ducts. According to scientists, it is the latter factor that has the highest impact on the occurrence of oxidative stress. The inflammation originates from the previously referenced varicocele, incompletely eliminated infection foci (“smoldering” infections) or certain systemic diseases such as diabetes, etc. The scientists have come to this conclusion based on research showing that almost one third of infertile men had significantly increased inflammation. At the time of inflammation, the number of pro-inflammatory molecules (cytokines) in the urogenital ducts is increased.
“Presumably, as many as 80% of male infertility cases originate
from oxidative stress (Tremellen 2008).”
Cytokines are a type of proteins released by various cells. Their main function is regulatory, i.e. they regulate the activity of certain cells partaking in the inflammatory processes. In case of inflammation in the urogenital ducts, the number of cytokines, such as interleukins (IL) 1β, IL-6, IL-8, IL-12, and IL-18, and tumor necrosis factor (TNF) α increase. Scientific research shows that an increased quantity of interleukins 1-β, IL-6 and IL-8 raise the level of oxidative stress and reduce the sperm count, motility and vitality, which in turn have a direct impact on male fertility. Thus, inflammation marker detection tests are carried out rather often when investigating the causes of male infertility.
Impact of Oxidative Stress on Male Infertility
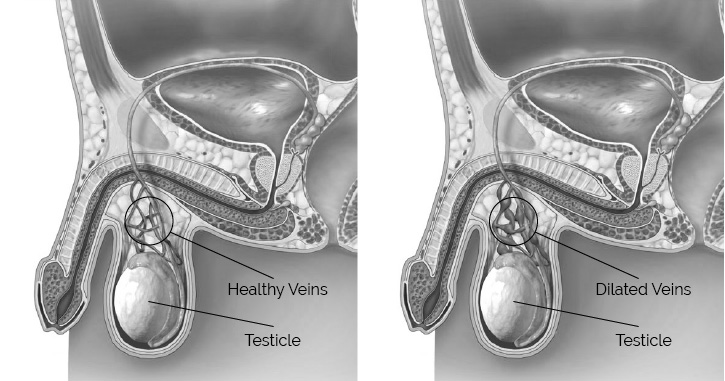
Free radicals are highly reactive molecules that can quickly react with lipids and proteins present in the membrane, thus damaging the walls of the spermatozoa. The damage to the sperm walls result in inferior motility, lower sperm count and second-rate appearance.
The damage caused by free radicals to sperm DNA is tremendous as DNA strands are especially susceptible to the process of oxidation. Sperm DNA may split or partially oxidize when affected by free radicals. Due to the detrimental effects of the free radicals, the DNA strand may lose its main function of carrying coded genetic information required for the replication of cells. Research shows that the DNA in approximately half of infertile men has been damaged.
A large scale scientific research analysis carried out in 2008 is the best clinical proof of the sperm DNA quality. It revealed a direct connection between sperm DNA damage and miscarriages. The more fragmented the sperm DNA strands, the more frequent the miscarriages.
Having taken the damage caused to the male reproductive function by oxidative stress into account, a large focus was given to antioxidants. In 2011, the Cochrane meta-analysis (scientific research analysis of great volume) was published presenting the analysis of the treatment of male infertility in almost 3000 couples by the use of antioxidants. The conclusions drawn in the analysis confirm that the use of antioxidants increase the pregnancy rate and number of live births for subfertile couples undergoing ART (assisted reproduction technology) cycles.
The review of the damage of oxidative stress reveals the latter as one of the main causes of male infertility. Oxidative stress is heavily influenced by poor daily habits and inadequate care of oneself. All the listed causes are dependent on the person himself, which gives rise to the hope that male infertility can be treated with a little bit of effort and time for oneself.
Analysis of Male Fertility Disorders
As there is a great variety of causes of male infertility, analyses and tests are imperative for their determination. The chapter is devoted to the review of the main recommended analyses, their importance, nominal values and deviations.
Semen Analysis
Semen analysis is the main test to be carried out and consists of the analysis of qualitative and quantitative parameters of semen (ejaculate). There are around ten parameters of semen; however, the main ones include volume (ml), sperm concentration (millions/ml), motility, morphology (sperm appearance is examined with a microscope) and the count of sperms with normal motility and appearance in percent.
| Parameter | Nominal value |
|---|---|
| Volume | >1.5 ml |
| Sperm concentration | >15 mln./ml |
| Progressive motility | >32% |
| Morphology (normal forms) | >4% |
The results of semen analysis and their conformity to the nominal values are assessed either by a medical specialist or calculated automatically via specialized software.
Following the tests, the assessed parameters are compared to nominal values and any deviations thereof are used to diagnose certain disorders (see Table 02).
| DIAGNOSIS | EXPLANATION |
|---|---|
| Oligozoospermia | When sperm concentration is < 20 million/ml. |
| Asthenozoospermia | Low progressive motility of spermatozoa |
| Aspermia | No ejaculate |
| Teratozoospermia | Insufficient number of spermatozoa with normal form (morphology) |
| Azoospermia | Insufficient count of mature spermatozoa |
Possible causes of oligozoospermia (decreased total sperm count) may vary significantly, starting with varicocele or prostatitis and ending with medication use. However, latent (“smoldering”) inflammations in the urogenital ducts remain one of the key reasons.
Asthenozoospermia (insufficient number of spermatozoa with progressive motility) along with teratozoospermia (Insufficient number of spermatozoa with normal morphology) may also be conditioned by oxidative stress, varicocele or hormonal imbalance.
Azoospermia is most often brought about by the obstruction of the vas deferens (ductus (vas) deferens).
The diagnosis may also possibly include more than one cause, e.g. oligoasthenoteratozoospermia, which signifies low sperm count (oligo-), motility impairment (astheno-) and low count of sperm with normal morphology (terato-).
DETERMINATION OF THE LEVEL OF OXIDATIVE STRESS IN SEMEN
Biochemical measures and special dye can help detect certain oxidation products in ejaculate, thus determining whether or not the semen is affected by oxidative stress.
The most accurate oxidative stress test currently available is a qualitative electrochemical test that measures sORP – Static oxidation-reduction potential in sperm, which is described as the balance between total oxidant and total reductant activity. Subfertile men have a significant imbalance in their sORP, and therefore can be distinguished by their sORP values from fertile men.
Up to 40% of men with impaired reproductive function have normal semen parameters, therefore standard semen analysis alone is insufficient for male infertility diagnosis. Since oxidative stress plays a large role in impaired male reproductive function, testing for seminal oxidative stress is included in the latest recommendations for male infertility diagnostics by the European Society of Human Reproduction and Embryology (ESHRE).
In case of positive results, causes of oxidative stress are looked into and adequate treatment is recommended.
Sperm DNA Fragmentation Assays
In some cases, one more important test known as sperm DNA fragmentation assay can be carried out to analyze male fertility causes in greater detail. The assay can be performed by several methods:
The assay can be performed by several methods:
The results of DNA integrity tests are measured by DNA fragmentation index (DFI) which is expressed in a percentage of sperm cells containing damaged DNA.
If the DFI is below 15%, it is considered insignificant and the probability of conception is high. However, if the DFI exceeds 30%, the probability of conception by natural means measures at barely several percent. Patients with high DFI are most often recommended to undertake ART procedures.
Comet method
DETERMINATION OF INFLAMMATORY MARKERS IN SEMEN
As observed in the earlier chapters, a large number of reported cases of male infertility were conditioned by inflammation. Hence, detection of inflammation using certain tests is a very important procedure to identifying causes of infertility.
These tests are categorized as biochemical, and they can be performed in a variety of ways. Usually, the patient’s blood or ejaculate is analyzed. In either of the cases, the inflammatory markers are assessed to see if they exceed the nominal value or not. An increase in the number of inflammatory markers shows inflammation in the urogenital ducts. If the marker count is exceedingly large, it is possible that the inflammation has been caused by an infection requiring the prescription of antibacterial treatment. In cases of small or average increase in inflammatory markers, the physician decides to either assign additional tests or start treatment.
Proper treatment with positive results ending in successful
conception of children can be assigned, provided that the
necessary tests are performed and the underlying cause of
infertility is determined.
Apart from the listed analyses, males can also undergo tests of hormone levels in blood (e.g., testosterone, luteinizing hormone (LH) or follicle-stimulating hormone (FSH)).
Proper treatment with positive results ending in successful conception of children can be assigned, provided that the necessary tests are performed and the underlying cause of infertility is determined.